Frailty is a geriatric condition associated with adverse health outcomes. Our study showed that physical inactivity in men and women, as well as dissatisfaction with social networks in women were associated with the development of frailty over 11-years. Moreover, results indicated that the combination of frailty risk factors was associated with an increase in frailty risk.
Frailty, characterized by fatigue, loss of appetite, functional difficulties, weakness, and low physical activity, is associated with numerous adverse health outcomes (e.g. mortality, falls, institutionalization). Consequently, it is one of the most severe health issues of older age and a major public health problem (1, 2). Studies have confirmed that physical activity (PA) (3, 4), nutritional factors (5) and social networks (6), are factors that play a role in the aetiology of frailty. Therefore, multicomponent interventions consisting of physical activity (endurance, strength and balance training), nutritional (sufficient protein intake) interventions as well as those focusing on maintenance of social networks are recommended in order to prevent the onset of frailty (7, 8).
Evidence pointing to the potential modifying effects of these interventions often stems from cross-sectional studies, while longitudinal studies examining the long-term effects are largely missing. Given this paucity of data, our study aimed to assess the modifying effects of physical activity, protein intake and satisfaction with one’s social network in a European based cohort with an 11-year-follow up. Additionally we aimed to assess the combination of these factors and how they impact the incidence of frailty.
In order to provide answers to our questions, the data from the Survey of Health, Ageing and Retirement in Europe (SHARE) were used. All in all, we included 22 226 community-dwelling persons aged ≥50 years, from 11 different countries. These people were considered to be robust or prefrail according to the ‘Frailty Instrument for Primary care of the Survey of Health, Ageing and Retirement in Europe’ (SHARE-FI), which is a validated sex-specific calculator, developed within the SHARE study, providing a score that allows classification of frailty (9). Additionally, self-reported physical activity (PA), protein intake and satisfaction with one’s social network were assessed. For our statistical analysis, we used cox regression models to calculate the impact of these parameters on the development of frailty within 11 years. As age, education, clinical & lifestyle factors (smoking, alcohol, BMI, depression, and long-term illness) have also an impact on the development on frailty, we have taken these as confounders into account.
The results of our study show that not performing regular PA, was associated with a higher risk of becoming frail during 11 year follow up when compared to performing PA regularly. Results can be seen in table 1. Overall, there were more than double the men and women who didn’t do regular PA developing frailty compared to those who did regular PA. These results are also underlined with the values of higher hazard ratios, showing that men who report no regular PA had an approximately twofold higher risk of developing frailty compared to those who report regular PA. In women the risk was somewhat lower but the results also indicate a higher risk for women not engaging in regular PA. In women the risk is somewhat lower but the results also indicate higher risk for women not engaging in regular PA. Although we observed slightly more men and women who reported low protein intake developing frailty, this was not found to be significantly associated with risk of developing frailty. Finally, the satisfaction with social network also had an impact on the development of frailty, however only in women. In men, we did not observe such an association.
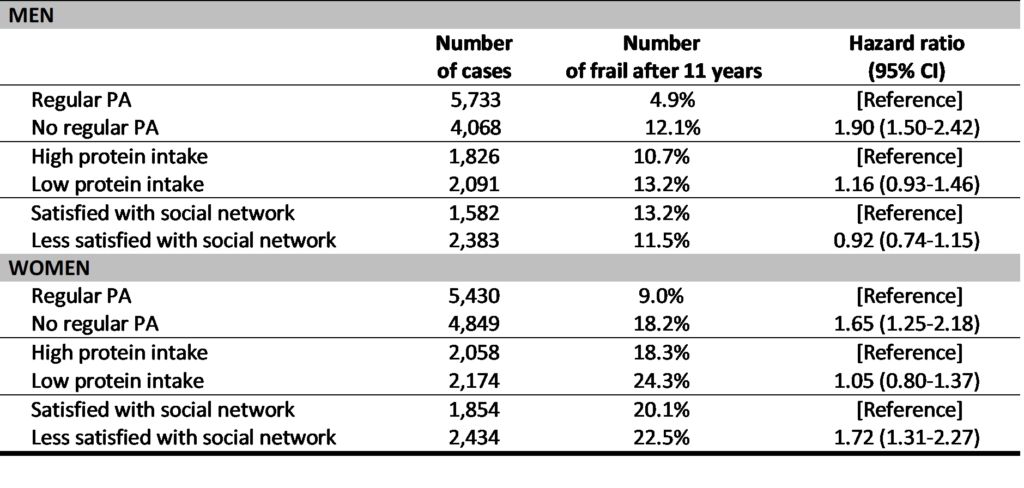
Note: Here you can see the adjusted hazard ratios for the risk factors that we analysed (not doing regular PA, low protein intake and low satisfaction with social network). Hazard ratios allow us to estimate the probability of an event (in our case frailty) happening between groups. Hazard ratios higher than 1.0 mean that there is more probability (risk) of something happening, while those lower than 1.0 mean there is a lower risk. For example in men who do not perform regular PA the hazard ratio of 1.90 means there is 1.90 times higher risk of frailty developing compared to those who do regular PA. Adjusting means that when we did these calculations we considered a variety of factors that could potentially influence the results (here we adjusted for age, education, smoking, alcohol consumption, body mass index, depression, long-term illness, as well as vigorous PA, protein intake and satisfaction with social network).
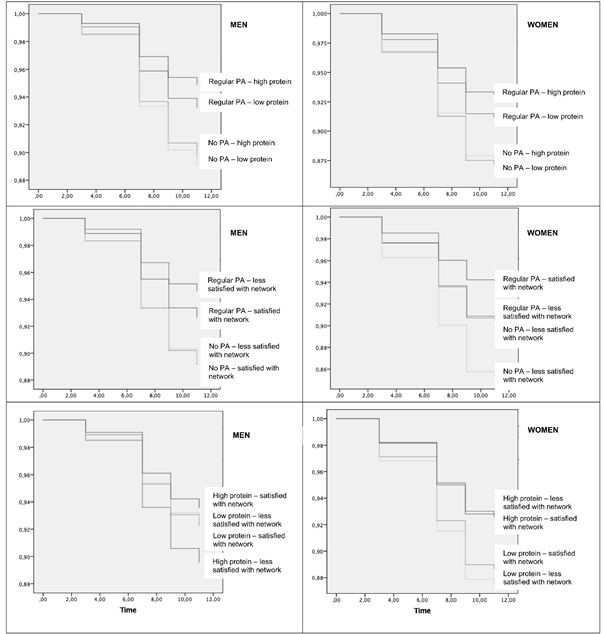
Furthermore, we also analysed to see if having a combination of two of these risk factors would also be associated with higher risk of frailty (figure 1). We observed the highest risk in women who reported social network dissatisfaction and not doing regular PA (HR= 2.58; 95%CI 1.71-3.90), in men the risk was also increased but somewhat lower (HR= 1.48; 95%CI 1.08-2.04). Highest risk for men was seen in those who did not engage regular PA and reported low protein intake (HR= 2.20; 95%CI 1.84-2.63), in women risk was also higher (HR= 1.94; 95%CI 1.28-2.91). The combination of low protein intake and dissatisfaction with the social network in men was not significant (HR=1.18; 95%CI 0.85-1.64), however, the same combination was found to be significant in women who had low protein intake and were dissatisfied with the social network (HR=1.73; 95%CI 1.19-2.53). These results were also adjusted for a number of factors, including: age, education, smoking, alcohol consumption, body mass index, depression and long term illness.
In the end, we can say that our study underlines the importance of regular PA foremost, but also of social network in frailty prevention, while low protein intake alone was not found to be associated with risk of frailty. Our results suggest that regular PA is the greatest modifying factor for development of frailty. Furthermore, we showed that a combination of two of these individual risk factors leads to more risk of frailty. In terms of prevention, we can say that in order to reduce the occurrence of frailty in our communities, interventions based on improving physical activity are very important, but we also need to consider that other factors contribute to the risk. Therefore, a broader approach is necessary for improving physical activity, social networks and protein intake.
References
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. The journals of gerontology Series A, Biological sciences and medical sciences. 2001;56(3):M146-56.
- Grabovac I, Haider S, Mogg C, Majewska B, Drgac D, Oberndorfer M, et al. Frailty Status Predicts All-Cause and Cause-Specific Mortality in Community Dwelling Older Adults. J Am Med Dir Assoc. 2019;20(10):1230-5 e2.
- Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA. Updating the Evidence for Physical Activity: Summative Reviews of the Epidemiological Evidence, Prevalence, and Interventions to Promote “Active Aging”. The Gerontologist. 2016;56 Suppl 2:268-80.
- McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016;17(3):567-80.
- Artaza-Artabe I, Saez-Lopez P, Sanchez-Hernandez N, Fernandez-Gutierrez N, Malafarina V. The relationship between nutrition and frailty: Effects of protein intake, nutritional supplementation, vitamin D and exercise on muscle metabolism in the elderly. A systematic review. Maturitas. 2016;Epub ahead of print.
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
- Lorenzo-López LM, A.; de Labra, C.; Regueiro-Folgueira, L.; Rodríguez-Villamil, J.L.; Millán-Calenti, J.C. Nutritional determinants of frailty in older adults: A systematic review. BMC Geriatrics. 2017;17(108).
- World Health Organization. Global Recommendations on Physical Activity for Health 2011 [Available from: http://www.who.int/dietphysicalactivity/factsheet_recommendations/en/.
- Romero-Ortuno R, Walsh CD, Lawlor BA, Kenny RA. A frailty instrument for primary care: findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). BMC geriatrics. 2010;10:57.
About the authors:

Sandra Haider, Department of Social and Preventive Medicine, Centre for Public Health, Medical University of Vienna, Austria

Igor Grabovac, Department of Social and Preventive Medicine, Centre for Public Health, Medical University of Vienna, Austria

Thomas Ernst Dorner, Department of Social and Preventive Medicine, Centre for Public Health, Medical University of Vienna, Austria
The article is based on:
Haider S, Grabovac I, Drgac D, Mogg C, Oberndorfer M, Dorner TE. Impact of physical activity, protein intake and social network and their combination on the development of frailty. Eur J Public Health. 2019 Oct 26. pii: ckz191. doi: 10.1093/eurpub/ckz191. [Epub ahead of print]










Leave A Comment